Learn what gestational diabetes is, proven tips for diet, exercise, and treatment to keep you and your baby healthy.
Introduction
When you’re pregnant, screening for gestational diabetes is one of those milestones you’ll encounter. You might ask yourself: Why do I have to drink this syrupy, sugary drink? What IS gestational diabetes, and should I be worried?
Gestational diabetes is a type of diabetes (high blood sugar) that develops during pregnancy. It’s caused by insulin resistance triggered by hormones from the placenta.
If you’re diagnosed, you may wonder: Why me? Sometimes, the diagnosis comes without warning or symptoms. The good news—it’s common, manageable, and often controlled through diet and exercise.
In this article, you’ll learn:
- What gestational diabetes is
- Risk factors
- How to manage it through diet and exercise
- Tips for a healthy pregnancy
What Is Gestational Diabetes?
Gestational diabetes is a type of diabetes that develops during pregnancy, usually diagnosed in the second trimester between weeks 24–28. However, if you’re at high risk—such as having had it in a previous pregnancy—you may be screened earlier.
It’s different from type 1 and type 2 diabetes because it usually goes away after pregnancy. However, having it increases your risk of developing type 2 diabetes later in life (1).
Gestational diabetes often occurs when hormones from the placenta block insulin’s action, causing insulin resistance.
Insulin is a hormone that helps lower blood sugar by allowing your cells to use glucose for energy. When you have gestational diabetes, your blood sugar remains higher than normal.

Did I Cause My Gestational Diabetes?
No—you didn’t cause it! There’s often no clear reason why it develops, and it’s not a reflection of something you did wrong. You can blame your pregnancy hormones for this one.
Risk Factors
While there’s nothing you did to cause gestational diabetes, certain factors can increase your risk (2):
- Family history of diabetes
- Previous pregnancy with gestational diabetes
- Being overweight before pregnancy
- Age 35+
- Certain ethnic backgrounds (Asian, Black, Hispanic/Latina, Native American)
Possible Effects on You and Your Baby
If untreated, gestational diabetes can lead to:
For the baby (3):
- Macrosomia (high birth weight)
- Low blood sugar after birth
- Jaundice
For the mother:
- Preeclampsia (high blood pressure in pregnancy)
- Increased risk of C-section
- Greater risk of type 2 diabetes later in life
With proper education, monitoring, and care, these risks can be reduced.
Screening and Diagnosis
Most women are screened for gestational diabetes in the second trimester using a Glucose Challenge Test (GCT):
- Drink a sweet glucose beverage
- Have your blood sugar checked one hour later
If your GCT result is high, you’ll have a Glucose Tolerance Test (GTT), which involves:
- Drinking a larger glucose beverage
- Having your blood sugar checked over several hours (4)
GCT results:
- Below 140 mg/dL → pass
- Above 140 mg/dL → move on to 3-hour GTT
GTT diagnostic criteria:
Gestational diabetes is diagnosed if at least two results exceed the normal range:
| Time after glucose drink | Normal Range |
|---|---|
| Fasting | <95 mg/dL |
| 1 hour | <180 mg/dL |
| 2 hours | <155 mg/dL |
| 3 hours | <140 mg/dL |
Managing Gestational Diabetes with Diet
The goal is to keep blood sugar within a healthy range by following a carbohydrate-controlled diet balanced with lean proteins and healthy fats.
Carbohydrates are the main nutrient that will raise your blood sugars. Learning the sources of carbohydrates is the first step in managing gestational diabetes with diet.
Carbohydrates are found in grains, bread products, beans, fruits, milk, yogurt, starchy vegetables, candy, pastries, cookies, ice cream, cakes and sugary beverages. Opt for complex carbohydrates vs. simple carbohydrates for the best blood sugar response.
Complex carbohydrates come from whole foods, are less processed and contain fiber. Simple carbohydrates are more processed, refined, and can be high in added sugars.
You may be asked to count your carbohydrates at each meal and snack. Spread out carbohydrates throughout the day between 3 meals and 2-3 snacks.
Carbohydrate Goals (per day: ~175g (5)):
- Breakfast: 30g
- Snack: 15g
- Lunch: 45g
- Snack: 15g
- Dinner: 45g
- Snack: 15g
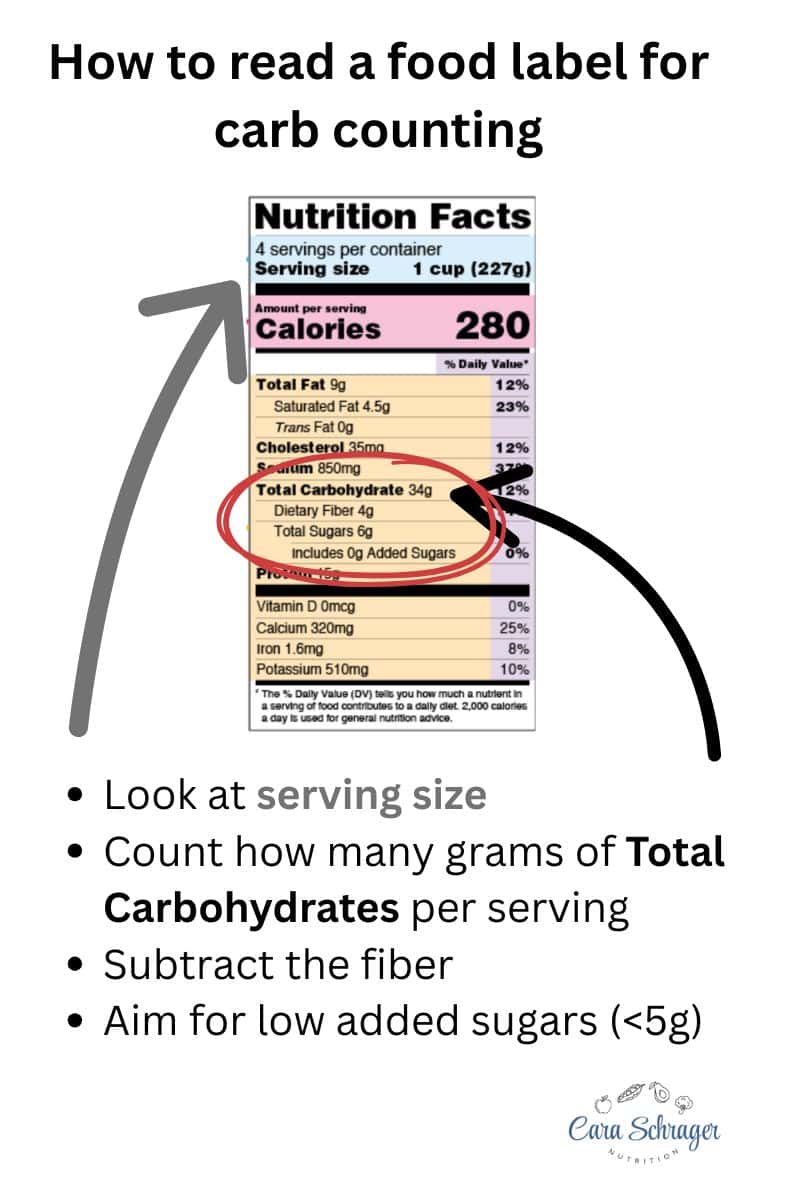
How to Count Carbohydrates
- Read food labels — check serving size and total carbs
- Subtract fiber from total carbs
- Measure portions
- Use apps like MyFitnessPal or CalorieKing
Breakfast Ideas (limit carbs to ~30g)
- 1 slice whole wheat toast with peanut butter + 1 flavored Greek yogurt with hemp seeds
- ½ cup cooked oatmeal with almond butter, chia seeds, and ½ cup blueberries
- 1 whole wheat English muffin with 1–2 eggs, avocado, and cheese
Lunch Ideas
- Peanut butter & sugar-free jelly on whole wheat bread, cheese stick, carrots with ranch dip
- Grain bowl with ½ cup beans, ⅔ cup brown rice, chicken, spinach, tomato, cucumber, cheese, and low-sugar dressing
- Avocado multigrain toast (1 slice) with egg salad + 1 small apple with almond butter
Dinner Ideas
- 1 cup cooked chickpea pasta with marinara, turkey meatballs, zucchini, and broccoli
- 1 small sweet potato with grilled chicken, asparagus, and side salad
- Salmon with 1 cup cooked quinoa and broccoli
Dessert Ideas
- Chia chocolate pudding with almond milk (recipe)
- 1 oz dark chocolate with ⅔ cup berries
- Almond flour cookies (recipe)
- Sugar-free whipped topping with strawberries
- Yasso Greek Yogurt Bar
Exercise and Physical Activity
Exercise can help lower blood sugar after meals.
- Aim for: 15-minute walk after each meal
- Other safe options: swimming, prenatal yoga (6)
High-intensity exercise may cause a temporary rise in blood sugar due to adrenaline release, but overall it supports better blood sugar control throughout the day (7).
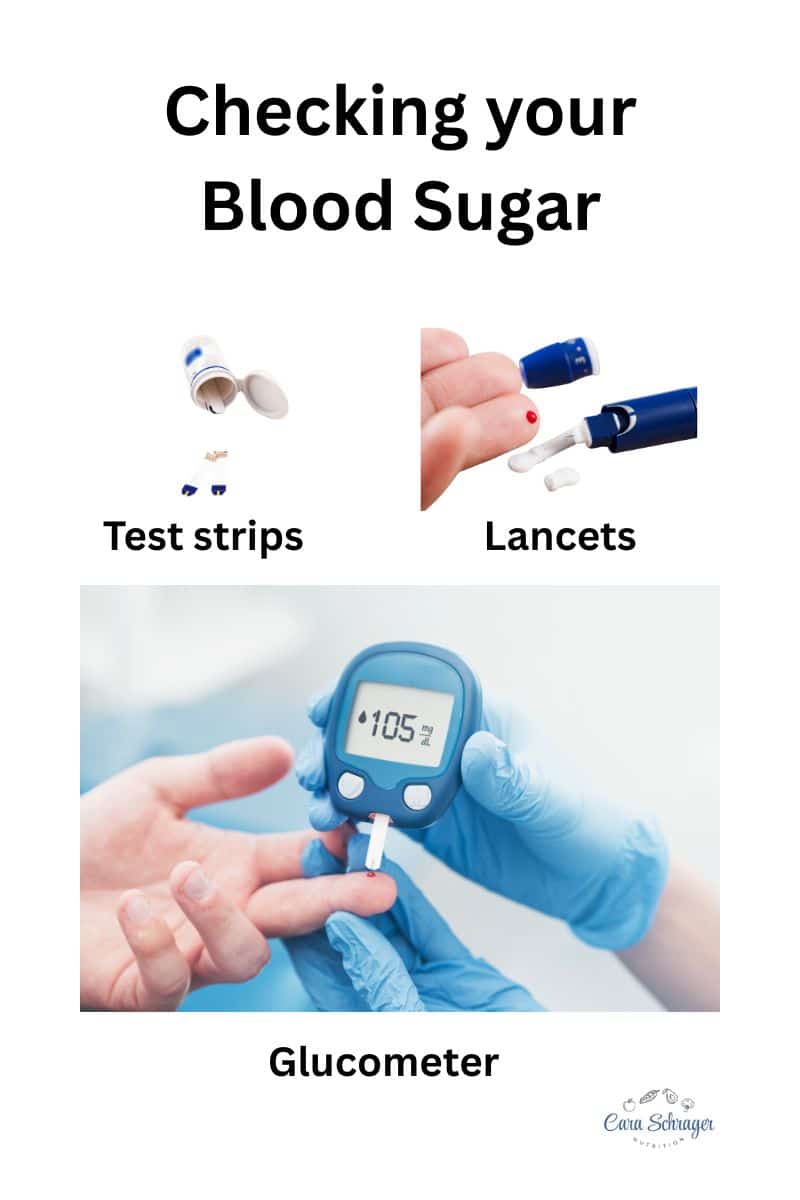
Blood Sugar Monitoring
You’ll likely check your blood sugar 4 times a day with a glucometer:
- Fasting (right after waking)
- 1 hour after each meal
Target Ranges (ACOG) (8):
- Fasting: <100 mg/dL
- 1 hour after meals: <140 mg/dL
- 2 hours after meals: <120 mg/dL
If Diet Isn’t Enough
Sometimes, following a gestational diabetes diet and exercise aren’t enough to keep blood sugar in range. In these cases, your provider may recommend insulin therapy.
- Insulin will not harm your baby
- It may be given at bedtime or before meals
- Your provider will guide you on how to administer it safely
After Giving Birth
Most women’s blood sugar returns to normal postpartum. However:
- Test your glucose 6–12 weeks after delivery
- Continue check-ups to monitor your risk for type 2 diabetes
- Meet with a registered dietitian to discuss prevention strategies
Tips for a Healthy Pregnancy with Gestational Diabetes
- Work closely with your healthcare team
- Keep a meal plan and glucose log
- Meet with a dietitian for individualized support
- Seek emotional and practical help—gestational diabetes can be overwhelming on top of preparing for a baby
Final Thoughts
Most women with gestational diabetes have safe, healthy pregnancies. While the diagnosis can feel frustrating, it’s manageable.
Monitoring your blood sugar, following a balanced diet, and staying active can help you meet your pregnancy nutrition needs while keeping blood sugars in range.
Work with a registered dietitian 1:1 to help you troubleshoot your meals to ensure you are meeting nutrition requirements for pregnancy, while keeping your blood sugars at their goal levels.
