Introduction
As a registered dietitian specializing in diabetes and insulin resistance, I’ve become increasingly curious about how insulin resistance plays a role during perimenopause.
Your 40s “era” (are we still saying era?) often comes with empowerment, career moves, and confidence — until hormones decide to shake things up. Many women notice a sudden shift in metabolism, partly due to changes in estrogen that influence insulin sensitivity, weight gain, and blood sugar control.
Perimenopause is the transitional phase before menopause — the point when menstrual cycles permanently cease. This stage is marked by significant hormonal changes. And since insulin itself is a hormone, it makes sense that it would have a major influence during this time.
Hormonal shifts bring big changes in metabolism. Insulin, produced by the pancreas, regulates blood sugar by helping glucose enter our cells for energy. During perimenopause, declining estrogen levels can reduce insulin sensitivity, making blood sugar harder to manage.
In this post, we’ll cover what causes these hormonal shifts, how to recognize the signs, and practical nutrition and lifestyle strategies to help you navigate this next phase.
What Is Insulin Resistance?
Insulin is a hormone produced by the beta cells in the pancreas that allows glucose to enter cells for energy. Insulin resistance occurs when cells don’t respond properly to insulin, leading to elevated blood sugar. It’s a major risk factor for type 2 diabetes.
The primary drivers of insulin resistance include physical inactivity and excess body fat, especially visceral fat (fat stored around the abdomen). Other contributing factors include genetics, dietary habits, certain medical conditions, and age.
Early warning signs may include:
- Energy crashes
- Sugar cravings
- Weight gain around the midsection
- Difficulty losing weight
- Elevated fasting glucose or A1C
Why Insulin Resistance Increases During Perimenopause
During perimenopause, estrogen levels decline — and estrogen plays a key role in insulin sensitivity (1). Here’s why insulin resistance tends to increase during this time:
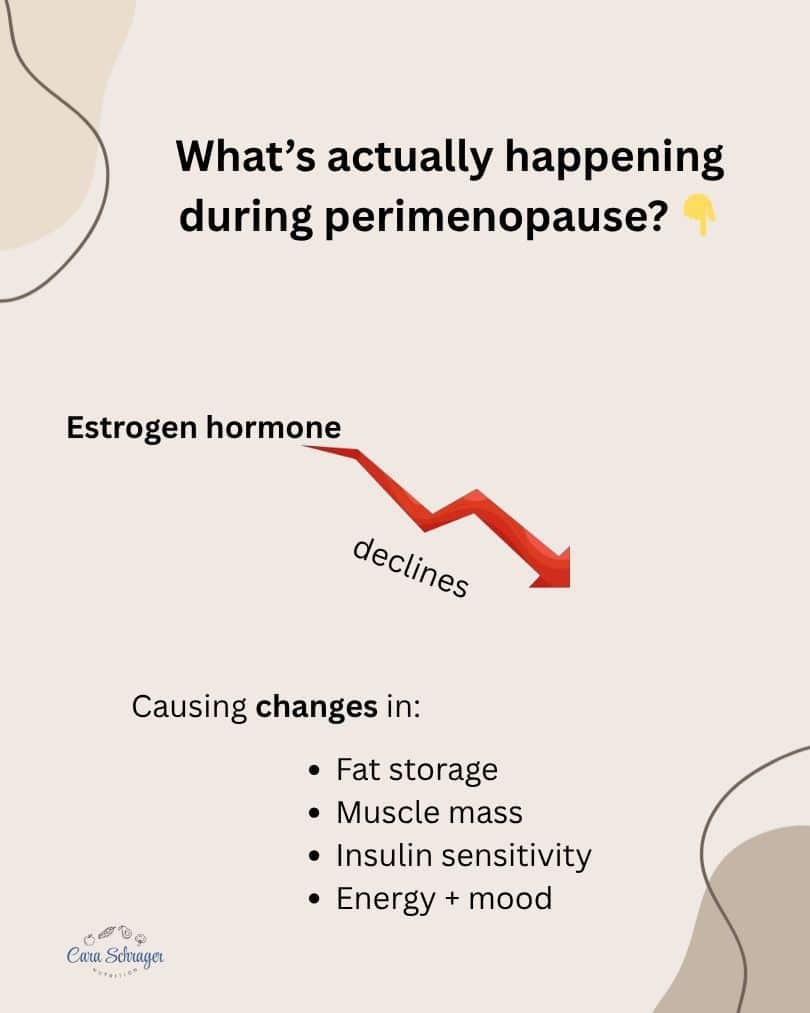
Hormonal factors
- Estrogen decline affects how the body stores fat and uses glucose.
- Progesterone fluctuations influence appetite and cravings.
- Body composition shifts: Less muscle mass and more visceral fat increase insulin resistance.
- Sleep and stress: Elevated cortisol worsens insulin resistance (2).
- Lifestyle changes: Less activity, irregular eating patterns, and chronic stress all contribute.
Nutrition Strategies to Support Insulin Sensitivity
1. Prioritize balanced meals
Include a combination of lean protein, complex carbs, and healthy fats:
- Protein: Skinless poultry, eggs, Greek yogurt, cottage cheese, fish, tofu, legumes, lean beef, ground turkey
- Complex carbs: Beans, lentils, whole grains, fruit
- Healthy fats: Nuts, nut butters, olive oil, avocado, seeds
Example meal: Quinoa bowl with grilled chicken, roasted vegetables, black beans, and avocado.
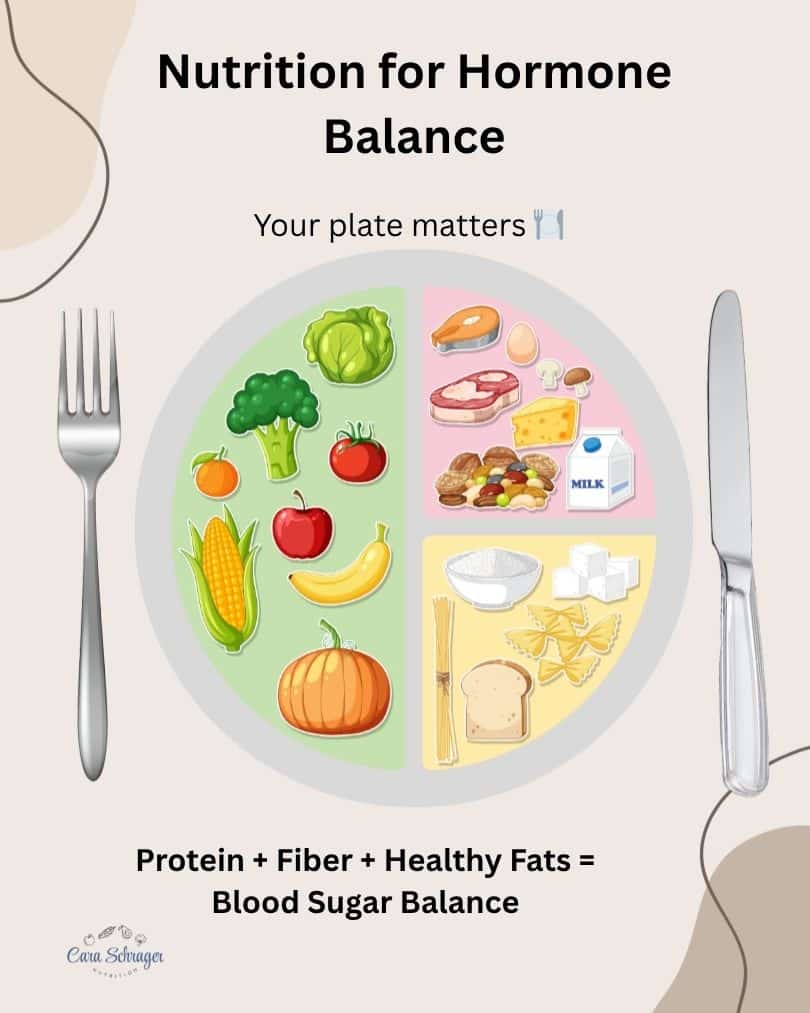
2. Focus on fiber
Soluble fiber (found in oats, beans, lentils, and berries) helps regulate blood sugar, feed gut bacteria, and lower cholesterol. Insoluble fiber supports regular digestion. A high fiber diet can help reduce constipation in perimenopause.
Choose low–glycemic index carbs such as whole grains, beans, and starchy vegetables instead of refined options like white bread or pasta.
3. Include high-quality protein
Protein helps maintain lean muscle, increases satiety, and stabilizes blood sugar throughout the day.
4. Support gut and metabolic health
In addition to fiber, incorporate fermented foods (like yogurt, kefir, sauerkraut, or kimchi) and prebiotics to reduce inflammation and support metabolic health.
5. Stay hydrated and limit alcohol
Alcohol can cause blood sugar fluctuations, disrupt sleep, and raise cortisol levels — all of which can worsen insulin resistance.
Lifestyle Strategies Beyond Nutrition
1. Exercise for Perimenopause and improve insulin sensitivity
Because declining estrogen accelerates muscle loss, strength training is key to preserving lean mass and improving insulin sensitivity.
You don’t need a gym membership — try YouTube classes, fitness apps, or local group sessions. Having an accountability partner helps with consistency!
Aerobic exercise (walking, running, biking, swimming, tennis) improves how your cells use glucose. Research shows that insulin sensitivity can remain elevated for up to 16 hours after exercise (3).
2. Prioritize sleep hygiene
Poor sleep increases cortisol, worsening insulin resistance. Aim for 7–9 hours of quality sleep.
Helpful habits:
- Try magnesium supplementation (if approved by your provider)
- Exercise regularly
- Avoid alcohol, heavy meals, or screens close to bedtime
3. Manage stress
Chronic stress raises cortisol, which inhibits insulin action and promotes glucose production (4).
Stress eating is common during hormonal transitions. Instead, explore stress management tools such as mindfulness, journaling, yoga, or nature walks.
4. Stay on top of lab work
Don’t skip your doctor visits! Regularly monitor fasting glucose, insulin, A1C, and lipid levels. Discuss your results with your healthcare provider or a registered dietitian (hi!).
Practical Tips for Everyday Life
Meal prep for balance
- Keep hard-boiled eggs ready for quick protein
- Pre-chop veggies for snacks
- Batch-cook whole grains like quinoa or farro
Smart snacking
Pair protein + fiber for steady energy.
Examples:
- Greek yogurt + berries
- Apple + nuts
- Hummus + veggies
Start small
Choose 1–2 goals that are specific, measurable, attainable, realistic, and time-bound (SMART).
Example: “I’ll add strength training twice a week on Tuesdays and Thursdays for 30 minutes.”
When to Seek Professional Support
If you’re unsure whether your current habits support your changing hormones, consult a registered dietitian. Personalized nutrition can make a tremendous difference — and it’s often covered by insurance.
Whether you’re already in perimenopause or preparing for it, it’s never too late to make proactive changes.
Final Thoughts
Aging is inevitable — but struggling through hormonal changes doesn’t have to be. Insulin resistance during perimenopause is common, but manageable with consistent, realistic nutrition and lifestyle shifts.
Take charge of your health and embrace this next chapter with confidence. Book a nutrition consultation to learn how to balance your hormones, support your metabolism, and feel your best.
